Intuitive Eating for Diabetes: An In-Depth Guide
Written by Isabel Vasquez RD, LDN
A lot of Latines worry about developing a chronic disease, especially type 2 diabetes and high cholesterol. When it comes to preventing or treating these conditions, nutrition is an important component. However, it’s easy to get caught up in restriction and food fear.
In our work as Latina registered dietitians, we hear a lot of clients say they’ve been given a long list of foods to avoid by other healthcare providers that they don’t even eat in the first place.
Maybe that’s happened to you. Or maybe you’ve been told to cut out your beloved cultural foods due to the misinformation out there on these foods’ health benefits. Let’s be real, the dishes we often see touted as “health-promoting” or good for blood sugar control are not culturally inclusive.
Taking a non-diet approach to nutrition helps you connect to your body’s cues and preferences rather than external rules and restrictions central to diets. Taking this approach doesn’t mean that you can’t manage a chronic condition; in fact, it’s a research-backed way of doing so that’s also gentler and more sustainable.
In this blog, we’ll share how diabetes affects the Latine community, the benefits of intuitive eating for diabetes, how you can practice intuitive eating with diabetes, and more. Let’s get into it!
What Is Intuitive Eating?
Intuitive eating is a non-diet, weight-inclusive approach to nutrition made up of 10 principles. It’s rooted in connecting with your body’s cues rather than external rules and restrictions common in diet culture to guide eating and exercise.
The ten principles of intuitive eating are:
Reject the Diet Mentality
Honor Your Hunger
Make Peace With Food
Challenge the Food Police
Discover the Satisfaction Factor
Feel Your Fullness
Cope With Your Emotions With Kindness
Respect Your Body
Movement - Feel the Difference
Honor Your Health With Gentle Nutrition
These principles serve as a guide to improve your relationship with food, movement, and your body while promoting your overall health.
What Is Diabetes?
There are three types of diabetes: type 1 diabetes, type 2 diabetes, and gestational diabetes. In the rest of this blog, we’ll mostly focus on type 2 diabetes since it affects 90-95% of those with diabetes; however, here’s an overview of each type of diabetes.
Type 1 Diabetes
Type 1 diabetes is typically diagnosed in childhood and, per the CDC, it affects 5-10% of those with diabetes. It happens when your pancreas doesn’t produce insulin, potentially from an autoimmune reaction where your body mistakenly attacks normal cells.
This type of diabetes requires daily insulin use to manage blood sugars.
Type 2 Diabetes
Type 2 diabetes is commonly diagnosed in adults, although younger people can be diagnosed with it, too. It happens when your body doesn’t use insulin effectively, called insulin resistance.
Insulin helps move sugar from your blood into your cells for energy. With type 2 diabetes, blood sugars remain high because insulin isn’t doing its job well.
As we mentioned above, this type of diabetes affects 90-95% of those with diabetes, so it’s the most widespread type of diabetes by far.
Gestational Diabetes
Gestational diabetes is a type of diabetes that occurs during pregnancy. It often resolves after the baby is born, but it does increase the risk for you or your baby to develop type 2 diabetes later in life, per the CDC.
How Does Type 2 Diabetes Affect The Latine Community?
The Latine community has higher rates of type 2 diabetes than non-Hispanic whites, due in part to genetics. According to the CDC, 11.7% of Hispanic adults have been diagnosed with diabetes, compared to just 6.9% of non-Hispanic White adults.
Latine individuals in the U.S. face unique challenges when it comes to preventing and treating type 2 diabetes including low socioeconomic status, lack of educational materials in Spanish, and less access to high-quality healthcare.
Plus, the rate of uninsured Latines in the U.S. is 2.5 times higher than that of non-Hispanic White Americans. Latines are also more likely to lack transportation to healthcare services, according to a 2020 study evaluating data from 1997-2017.
Many of these factors are social determinants of health—”conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
If someone can’t take off work to get to a healthcare appointment or if they can make it but can’t find a provider who speaks their language, their health will suffer. Even if they do make it to the appointment and can communicate with ease, they may receive a list of foods to eat that aren’t culturally appropriate, leaving them feeling misunderstood and helpless.
Common Nutrition Interventions For Diabetes
When it comes to the management of type 2 diabetes through nutrition, there are a couple of foundational interventions.
Establish A Consistent Eating Pattern
Eating at consistent intervals throughout the day helps prevent the binge-restrict cycle which can cause hyperglycemia and hypoglycemia. Honestly, this intervention is helpful for most people, not just for those with diabetes.
When you eat, your blood sugars rise. That’s just a normal effect of eating. As your body digests the food over the course of a few hours, your blood sugars decrease until you eat again.
However, if you go too long between meals, they can drop too low, causing hypoglycemia (blood sugars below 70 mg/dL). Signs of hypoglycemia, per the CDC, include fast heartbeat, shaking, sweating, anxiety, irritability, dizziness, and hunger.
Therefore, eating at regular intervals is important to prevent hypoglycemia, which can backfire and lead to binge eating or eating far beyond comfortable fullness.
For all of us, promoting stable blood sugars generally translates to consistent energy and concentration levels. So, eating at regular intervals throughout the day is helpful.
Add Nutrition to Your Meals
Incorporating a variety of food groups in your meals and snacks can also help prevent blood sugar spikes and drops.
There is a lot of fear-mongering about carbs in our society as a whole right now, but especially in the context of diabetes. People may believe the myth that they have to cut out carbs to manage diabetes, but that’s generally not the case.
For one, the type of carbohydrates you have matters. Some carbohydrates, like beans, fruits, and root vegetables, are also high in fiber which helps mitigate the carbs’ impact on blood sugars.
You can also pair carbohydrates with protein, fat, and other sources of fiber to prevent rapid blood sugar spikes. These other food groups are generally digested slower by our bodies, so they reduce the rate at which blood sugars rise after eating and prevent rapid drops upon digestion.
With any of these interventions, it’s important to monitor your blood sugars to see how what you eat, how much you eat, and when you eat impact your blood sugars with diabetes. Everyone’s body is different, so connect with your body to see how it responds.
Also, remember that there’s more to diabetes management than just nutrition. Diatribe has a great list of 42 factors that affect blood glucose. We are often quick to blame food, but there could be something else impacting your blood sugars like stress, medication, or exercise.
Benefits Of Intuitive Eating For Diabetes
Intuitive eating is associated with a bunch of health benefits including improved cholesterol levels, lower rates of disordered eating, increased self-esteem, and better blood pressure.
When it comes to diabetes, research shows some specific benefits of intuitive eating.
A 2016 study (CW: weight stigmatizing language) found that participants in a 5.5-month-long training that included education on mindfulness-based eating had significantly lower fasting glucose levels than the control group at a 12-month follow-up.
The control group’s fasting glucose levels rose at the follow-up visit, so mindful or intuitive eating-based interventions may help prevent these increases in fasting blood sugars over time.
Another study found that a mindfulness-eating-based program for type 2 diabetes was just as effective as a traditional diabetes self-management education program at reducing hemoglobin A1C (a measure of average blood sugar levels over 3 months).
Finally, a 2021 observational study conducted in Brazil found that participants with type 2 diabetes who scored higher on an intuitive eating scale (a questionnaire measuring how aligned someone’s eating is with intuitive eating) had lower rates of inadequate glycemic control, regardless of their BMI.
For the record, intuitive eating isn’t just associated with better blood sugar management in people with type 2 diabetes. Studies have also shown that intuitive eating is associated with better glycemic control in adolescents with type 1 diabetes and in pregnant and postpartum women with gestational diabetes.
How To Practice Intuitive Eating With Diabetes
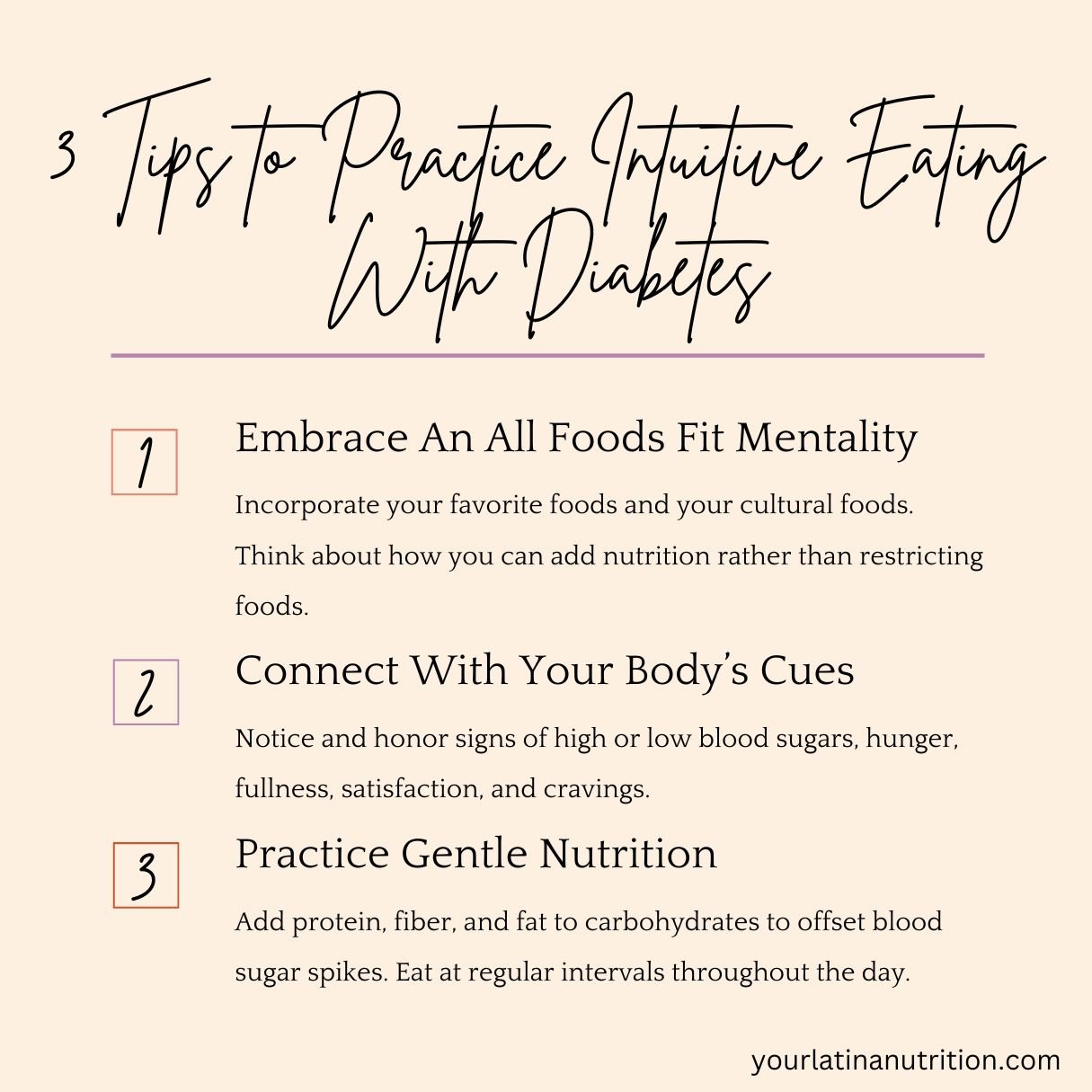
Embrace An All Foods Fit Mentality
Leaning into your food preferences and taking an “all foods fit” approach is central to intuitive eating. Find foods that you enjoy that are culturally relevant to you.
Forcing yourself to eat in a way that isn’t authentic to your preferences isn’t sustainable and takes the fun and pleasure out of eating. You can absolutely find pleasure in eating while also managing diabetes.
There are so many different ways of getting in nutritional variety, and there are plenty of Latine cultural foods that serve as sources of carbohydrates, protein, fat, and fiber. We have great nutritional variety in our meals, so lean into that.
For example, many Latin American countries eat root vegetables like plátanos, yuca, or yautia which are high in fiber to offset blood sugar spikes.
We also tend to eat a lot of beans, which provide not only carbs but also protein and fiber to balance blood sugars. The American Diabetes Association even considers beans a “superstar food” for diabetes because of their fiber, protein, and vitamin and mineral content.
You don’t need to cut out your cultural foods or your other favorite foods to manage your health. There are ways to incorporate both pleasure and health promotion in your food choices.
Connect With Your Body’s Cues
Leaning into your body’s cues is another central aspect of intuitive eating. This typically includes tuning in to your hunger and fullness cues, satisfaction and cravings, and other physical sensations.
For example, your eating pattern may impact your energy levels, concentration during work, or mood. If you’re going too long between meals you may have lower energy levels, struggle with concentrating, and feel irritable. Starting to notice these cues can help you understand your body better and honors its needs.
You may notice that when you eat nutritionally well-rounded meals you feel more energetic for longer. On the other hand, you may notice that when you cut out your favorite foods, your mind is consumed with thoughts about those foods.
Using interoception—the feeling of knowing what is happening in your body—can also help you notice when your blood sugars are off so you can take action to promote blood sugar regulation.
Practice Gentle Nutrition
Gentle nutrition is the tenth and final principle of intuitive eating. It invites you to incorporate satisfaction, pleasure, and nutrition into your food choices (read our blog post on gentle nutrition here!). We like to think of it as adding nutrition, rather than cutting out foods.
For diabetes, you can practice gentle nutrition by adding sources of protein and fiber to your meals while also incorporating carbohydrates you enjoy. Rather than thinking of what you need to restrict, think about what you can add to make it a more blood-sugar-friendly meal.
Consider the amounts and combinations of food you’re having to find a balance of both promoting your health and honoring your cravings and preferences.
Final Thoughts
Unfortunately, diet culture often makes us think we have to restrict food in order to promote our health. In reality, you can manage diabetes without getting caught in the diet mentality. In fact, intuitive eating is associated with positive effects on blood sugar and diabetes.
For education on how to ADD nutrition to your favorite Latine cultural dishes, make peace with food, and focus on your health without dieting, join our nutrition library for just $27/month.
If you liked this post, you may also like:
What is Gentle Nutrition? Plus 3 Tips to Get Started
Food Habituation: The Case for Eating Whatever You Want
Can I Manage My High Cholesterol With Intuitive Eating?
Disclaimer: This blog is for informational and educational purposes only. It isn’t a substitute for individual medical or mental health advice and doesn’t constitute a provider-patient relationship.